GI Intervention
News


GI Intervention
News
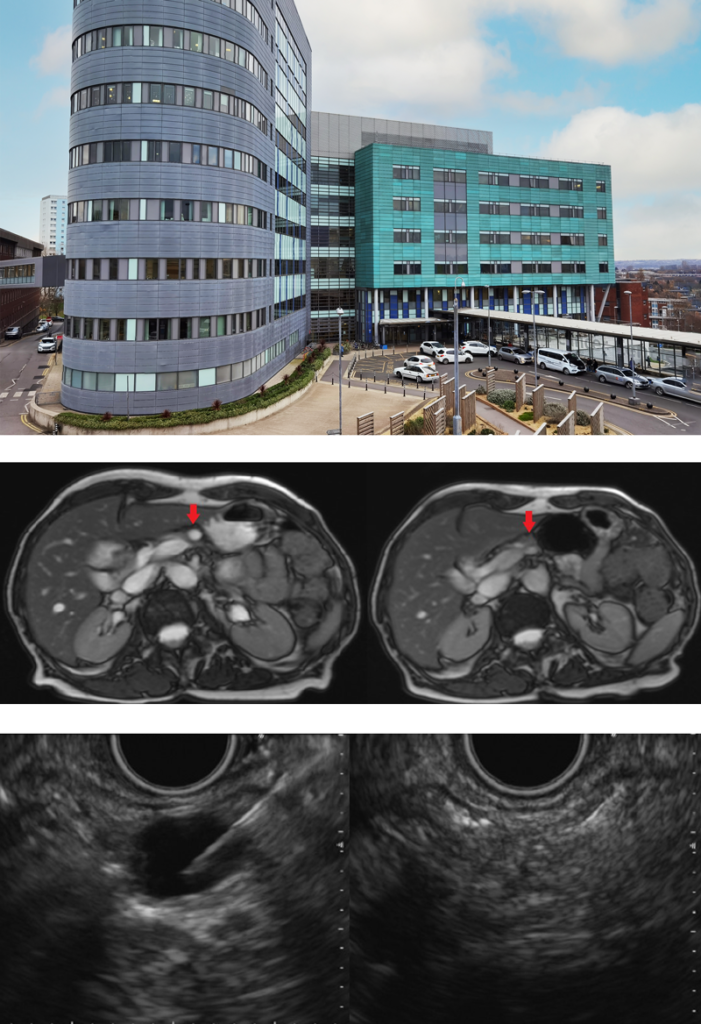
Treatment of pancreatic lesions using RFA in Leeds, St James’ University Hospital
Pancreatic cysts are common in the general population and are often discovered incidentally following abdominal imaging performed for other indications. These cysts have a pre-malignant potential and patients are subjected to longitudinal follow-up which can be associated with anxiety to the patient as well as growing costs to the National Health Service. Endoscopic ultrasound guided radiofrequency ablation (EUS-RFA) of these cysts is being studied as a treatment option of these pre-malignant cysts and if successful, may obviate the need for long-term follow-up. EUS-RFA of pancreatic cysts is being carried out at Leeds Teaching Hospitals NHS Trust and we are also involved in the RADIOCYST study, evaluating the safety and efficacy of EUS-RFA in these patients.
The EUSRA probe, in conjunction with a radiofrequency generator, from Taewoong Medical provides safe ablative treatment with focused application of controlled energy. Pre-set wattage and ablation time are used to control the volume to tissue to be ablated, thus preventing excess energy delivery. An inner cooling system with irrigation of cold saline acts as a safety mechanism to prevent overheating of the probe and excessive charring of the soft tissues. Complete ablation of the cyst is confirmed under EUS guidance.
We illustrate a case of a patient with a 12mm cyst in the body of the pancreas. EUS-RFA was performed, and the patient was discharged the next day following a period of observation. Interval scans showed progressive reduction in the size of the pancreatic cyst and a scan 3 years after her index scan showed complete resolution of the pancreatic cyst.
The use of EUS-RFA in pancreatic lesions also extends to treatment of neuroendocrine tumours, pancreatic cystic neoplasms and unresectable pancreatic adenocarcinoma. In patients whom surgery is precluded or deemed high risk, there may be a role for EUS-RFA in treatment of these lesions and further prospective studies are required to assess this.
Dr Matthew Huggett (Consultant Gastroenterologist and Hepatologist), Dr Wei On (Post CCT Fellow in PB Medicine and Endoscopy), Leeds Teaching Hospitals NHS Trust
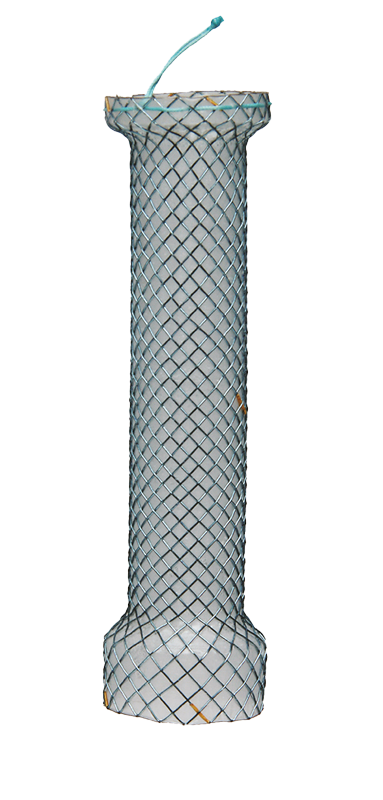
Expert Interview – Dr Marc Giovannini on the Giobor Stent
Dr. Marc Giovannini from Paoli-Calmettes Institute, France is well known as a pioneer in Endoscopic Ultrasound. He shares his experience with using the Giobor stent in this interview.
Interview with Dr Perminder Phull
We sat down with Dr Perminder Phull to get his opinion on using the proximal-release Cervical stent for the first time. Read about his experience below:
Why did you choose to use the Cervical stent, what features attracted you to using it?
To remove a proximally migrated stent embedded in upper oesophagus using the stent-in-stent technique; the original (Niti-S) stent had been placed to treat a distal oesophageal refractory post-radiotherapy stricture; patient was treated last year for oesophageal squamous cell cancer. Due to the location of the proximal end of the embedded stent being only a few cm distal to the cricopharyengeus, placement of a standard stent would not have been possible or tolerated by the patient.
What do you like about the stent? Any tips or tricks that you have learnt?
The deployment technique is slightly different to the Niti-S stent but still straightforward and managed without difficulty by nursing staff.
A brief summary of the results you have experienced so far?
This was a complex situation to manage, and it took 6 weeks to free up the impacted stent, with the cervical stent being replaced every 2 weeks.
What are your future plans for using the Cervical stent? E.g. will this become a routine tool for you to use to treat future cases?
Yes, this will become a standard stent for treating high oesophageal strictures.

PuraStat®: North-East Paves the Way for RAVE
Purastat is widely used in the UK, however with an ever-expanding range of indications and uses, Meet the Expert’s sessions aim to share best practice and experience amongst peers.
On this occasion Dr Leeds discussed the promising outlook of Purastat in treating duodenal EMRs, difficult lesions or ‘Absolute Bandit Territory’ as John aptly put it! The session presented case studies and live footage of duodenal EMR’s, with a detailed discussion from John’s extensive knowledge in this area.
Dr Hancock’s session told the story of how he began treating Radiation Proctopathy, also known as Radiation-Associated Vascular Ectasias (RAVE) with Purastat some years ago and was “astounded” by the results and the impact on quality of life. With some patients not being seen in clinic for several years now, to most recently reducing the number of blood transfusions required from 1-2 per month, to a stint of 4 months and counting without requiring further treatment.
Here’s what Dr Hancock had to say about Purastat:
“Not only is this a very, very easy-to-use, effective haemostatic agent but I think it has huge potential in all the work we do in so many different areas. From managing chronic inflammatory conditions like Chron’s fistulas, accelerating ulcer healing and preventing re-bleeding, you name it! Particularly for oesophageal strictures; I think there is huge potential for Purastat in endoscopy.”
If you’d like to host your own “Meet the Experts” session within your regional group we’d be happy to facilitate this for you. Get in touch at GI@aquilant.net.
Our ‘A week with’ series will be starting on Twitter this summer; first in the spotlight is Dr John Leeds, Consultant Pancreaticobiliary Physician, from Freeman Hospital. Please join us on Twitter to see a two-minute video each day, for 5 days to learn more about Dr Leeds, his practices and his ambitions.
Dr Leeds, Consultant Pancreaticobiliary Physician, Freeman Hospital
If you would like to take part in our ‘A week with’ series, then please contact us on gi@aquilant.net; we would love to hear from you!
Contact the Team





